30 Million Ghanaians, 80 Psychiatrists: Examining Ghana's Mental Health Gap

Table of Contents
The Stark Reality: A Critical Shortage of Mental Health Professionals
Insufficient Psychiatrists and Other Mental Health Workers
Ghana's mental health system is drastically understaffed. The ratio of psychiatrists to population is abysmal, with approximately one psychiatrist for every 375,000 people. This stark reality is further exacerbated by a shortage of other crucial mental health workers, including psychologists, counselors, and psychiatric nurses. Comparable nations in Africa and globally boast significantly higher ratios of mental health professionals per capita.
- Psychiatrists: Approximately 80 serving a population of over 30 million.
- Psychologists: Precise figures are difficult to obtain, but the number is far below what's needed for adequate coverage.
- Counselors: Similarly, a significant shortage exists, particularly in rural areas.
- Comparison: Developed nations often have ratios exceeding 1 psychiatrist per 10,000 people.
The geographical distribution of these professionals is also uneven, with a concentration in urban areas, leaving rural communities with minimal access to psychiatric care in Ghana. This disparity exacerbates existing inequalities and limits access for vulnerable populations.
Inadequate Infrastructure and Resources
Beyond the shortage of personnel, Ghana faces a critical deficiency in mental health infrastructure and resources. Many existing facilities are ill-equipped, underfunded, and lack the necessary resources to provide comprehensive care.
- Lack of Hospitals and Clinics: Many regions lack dedicated mental health hospitals or even clinics, forcing individuals to travel long distances for treatment.
- Limited Equipment and Supplies: Essential medications, diagnostic tools, and therapeutic equipment are often in short supply.
- Poor Funding: Inadequate government funding severely hampers the ability of existing facilities to provide quality care.
The impact on access to care, especially in rural areas, is devastating. Many individuals with mental health conditions go untreated, leading to worsening symptoms and potentially tragic outcomes.
Consequences of the Mental Health Gap in Ghana
Increased Stigma and Underdiagnosis
The shortage of mental health professionals in Ghana significantly contributes to the pervasive stigma surrounding mental illness. The lack of accessible care fosters fear and misunderstanding, leading to underdiagnosis and delayed treatment.
- Cultural Beliefs: Traditional beliefs and cultural practices often stigmatize mental illness, hindering individuals from seeking help.
- Fear of Discrimination: The fear of social isolation and discrimination prevents many from disclosing their struggles.
- Impact on Treatment: Delayed diagnosis and treatment result in poorer outcomes and increased suffering.
This stigma creates a vicious cycle, perpetuating the mental health crisis in Ghana and hindering progress.
Increased Burden on Families and Communities
The absence of adequate mental healthcare places an immense burden on families and communities who often shoulder the responsibility of caring for individuals with mental illness without professional support.
- Financial Strain: Families bear the cost of treatment, medication, and caregiving, often leading to financial hardship.
- Emotional Toll: The emotional and psychological impact on family members can be profound, leading to stress, burnout, and family conflict.
- Lack of Respite Care: Limited access to respite care services places further strain on caregivers.
This lack of support systems exacerbates the challenges faced by both individuals with mental illness and their families, perpetuating the cycle of suffering.
Economic Impact of Untreated Mental Illness
Untreated mental illness has a significant economic impact on Ghana, resulting in substantial losses in productivity, increased healthcare costs, and societal costs.
- Lost Productivity: Individuals unable to work due to untreated mental illness represent a significant loss of economic contribution.
- Healthcare Expenses: The indirect costs associated with managing untreated mental health conditions—including emergency room visits and hospitalizations—are substantial.
- Societal Impact: The social consequences of untreated mental illness, such as crime and social unrest, further burden the economy.
Addressing Ghana's mental health gap is not merely a humanitarian imperative; it is also a vital economic necessity.
Potential Solutions and Strategies to Bridge Ghana's Mental Health Gap
Investment in Training and Education
Addressing Ghana's mental health crisis requires a substantial investment in training and education to increase the number of qualified mental health professionals.
- Funding for Training Programs: Significant investment is needed to establish and support comprehensive training programs for psychiatrists, psychologists, and other mental health workers.
- Scholarships and Financial Aid: Providing scholarships and financial aid can attract and retain talented individuals in the field.
- International Collaborations: Partnerships with international organizations can provide valuable expertise and resources.
Improving the quality of mental health education is equally crucial, ensuring that professionals are equipped with the skills and knowledge needed to provide effective care.
Improved Infrastructure and Resource Allocation
The government must invest in building and improving mental health infrastructure, ensuring that facilities have the necessary resources to deliver quality care.
- Government Funding: Increased and sustained government funding is essential for building new facilities and expanding existing ones.
- Public-Private Partnerships: Collaborations with private organizations can leverage resources and expertise.
- International Aid: Seeking international aid and partnerships can provide much-needed support.
Providing better equipment, supplies, and technology is crucial for providing effective treatment and improving the quality of care.
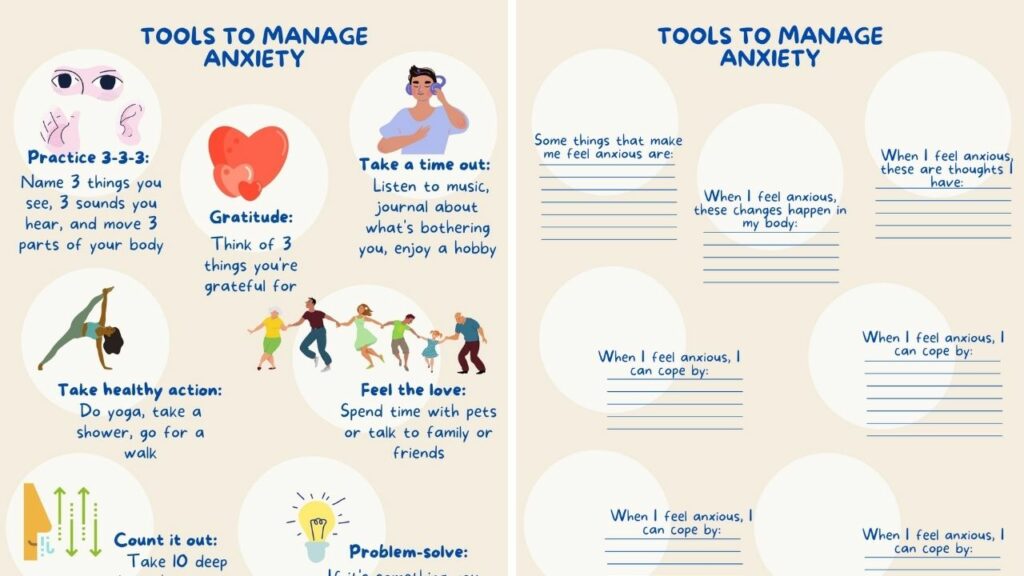
Addressing Stigma through Public Awareness Campaigns
Reducing stigma associated with mental illness is critical to encouraging help-seeking behavior. Comprehensive public awareness campaigns can play a pivotal role.
- Social Media Campaigns: Utilizing social media platforms can reach a wider audience and promote open discussion.
- Community Engagement: Engaging with communities to educate and address misconceptions is vital.
- Media Collaboration: Collaborating with media outlets to share accurate information and humanize the experience of mental illness can help combat stigma.
Through education and awareness, we can challenge negative perceptions and encourage those struggling to seek help.
Integration of Mental Health into Primary Care
Integrating mental healthcare into primary care settings can significantly improve access and reduce barriers to treatment.
- Training Primary Care Physicians: Equipping primary care physicians with the skills to screen for and manage common mental health conditions is crucial.
- Collaboration: Facilitating close collaboration between primary care and specialist mental health services ensures comprehensive care.
Conclusion
Ghana's mental health gap represents a profound crisis with far-reaching consequences for individuals, families, and the nation. The critical shortage of mental health professionals, inadequate infrastructure, and pervasive stigma contribute to underdiagnosis, delayed treatment, and immense suffering. Addressing this crisis requires a multifaceted approach involving increased investment in training and education, improved infrastructure and resource allocation, public awareness campaigns to combat stigma, and integration of mental health services into primary care. We must demand better mental health services from our government, support organizations working to improve mental healthcare access in Ghana, and donate to mental health charities in Ghana. Investing in mental health is an investment in Ghana's future – a future where every citizen has access to the care they need to thrive. Let's work together to bridge Ghana's mental health gap and build a healthier, more prosperous nation.

Featured Posts
-
 Australias Oppositions Plan A 9 Billion Budget Improvement Strategy
May 02, 2025
Australias Oppositions Plan A 9 Billion Budget Improvement Strategy
May 02, 2025 -
 Safeguarding Our Future Investing In Childrens Mental Health Now
May 02, 2025
Safeguarding Our Future Investing In Childrens Mental Health Now
May 02, 2025 -
 Public Opinion Divided The Rupert Lowe Controversy In Great Yarmouth
May 02, 2025
Public Opinion Divided The Rupert Lowe Controversy In Great Yarmouth
May 02, 2025 -
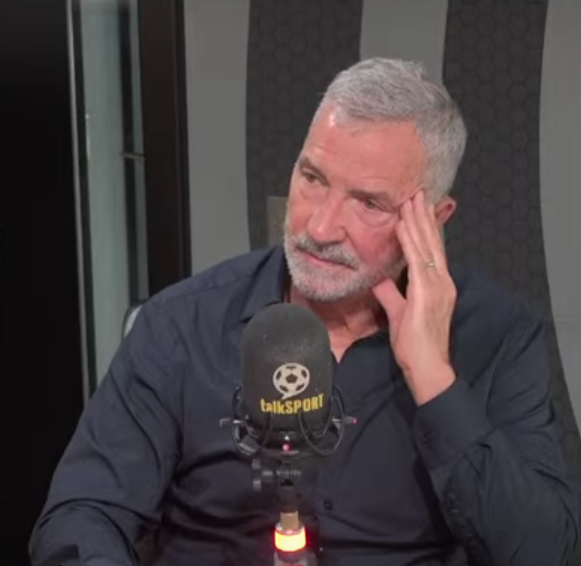 Declan Rice Souness Highlights Key Area For Improvement To Become World Class
May 02, 2025
Declan Rice Souness Highlights Key Area For Improvement To Become World Class
May 02, 2025 -
 Smart Ring Technology Addressing Cheating Concerns
May 02, 2025
Smart Ring Technology Addressing Cheating Concerns
May 02, 2025
Latest Posts
-
 Macron Remonte Par Sardou Le Diner Tendu
May 03, 2025
Macron Remonte Par Sardou Le Diner Tendu
May 03, 2025 -
 La Rencontre Trump Macron Au Vatican Contexte Et Consequences
May 03, 2025
La Rencontre Trump Macron Au Vatican Contexte Et Consequences
May 03, 2025 -
 Vatican Le Tu Ne Devrais Pas Etre Ici De Trump A Macron Decryptage
May 03, 2025
Vatican Le Tu Ne Devrais Pas Etre Ici De Trump A Macron Decryptage
May 03, 2025 -
 Patriotisme Economique Europeen Le Role De L Intelligence Artificielle Selon Macron
May 03, 2025
Patriotisme Economique Europeen Le Role De L Intelligence Artificielle Selon Macron
May 03, 2025 -
 Tensions Au Vatican Analyse De La Rencontre Trump Macron
May 03, 2025
Tensions Au Vatican Analyse De La Rencontre Trump Macron
May 03, 2025
