Combating Measles: Strategies To Overcome Persistent Infections
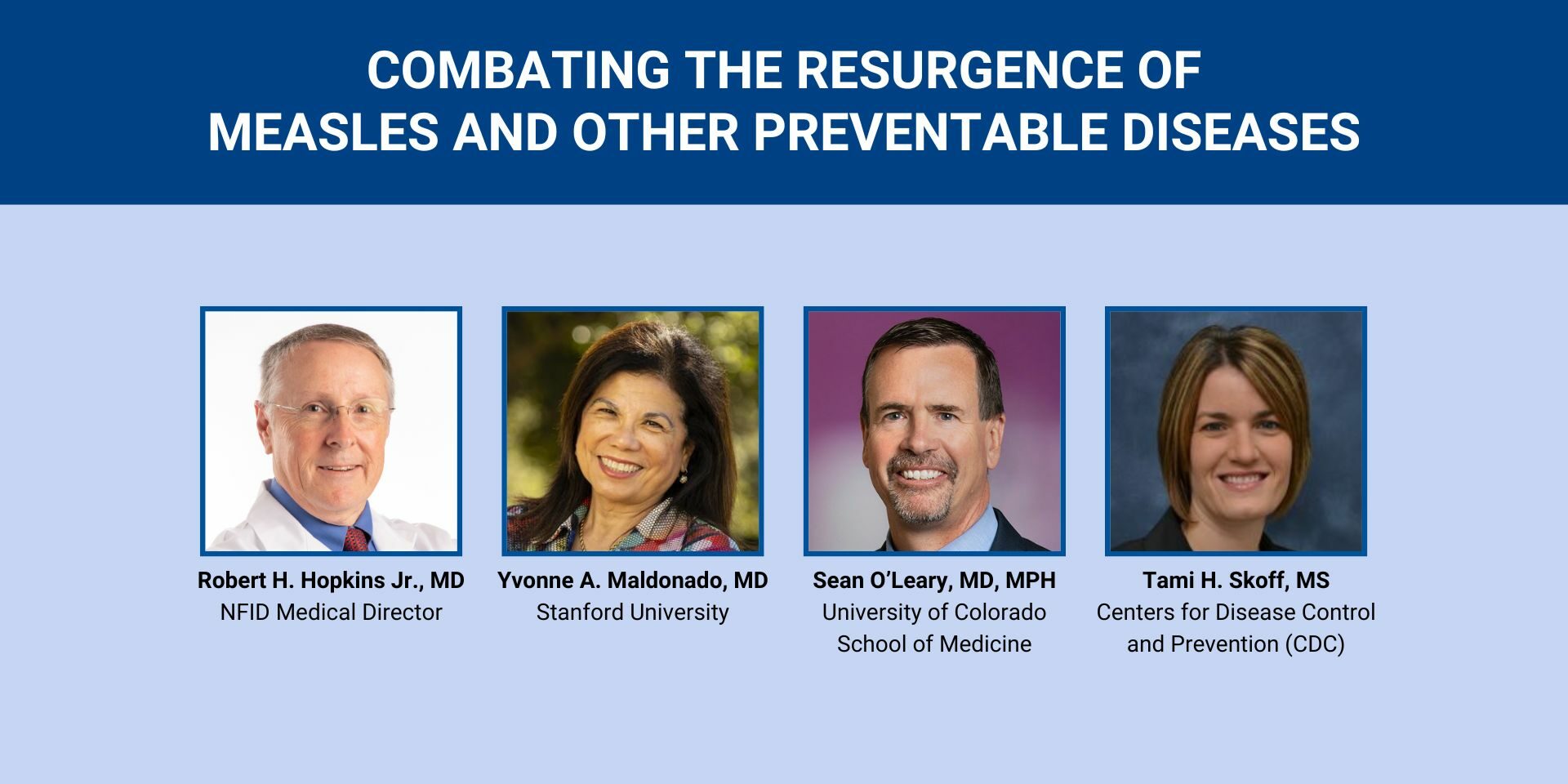
Table of Contents
Understanding Persistent Measles Infections
Defining Persistent Measles
What constitutes a persistent measles infection? It's not simply a prolonged rash. A persistent measles infection involves symptoms lasting significantly longer than the typical 7-10 days, often presenting with atypical characteristics. This can include:
- Recurrent fever: Episodes of high fever returning after an initial period of improvement.
- Prolonged rash: A measles rash that persists for weeks, potentially changing in appearance.
- Neurological symptoms: The development of symptoms affecting the brain and nervous system, such as seizures, encephalitis (brain inflammation), or ataxia (lack of muscle coordination).
- Giant cell pneumonia: A severe form of pneumonia characterized by the presence of large cells in the lungs.
It's important to distinguish between true persistent measles and complications that mimic persistence. Many cases of prolonged symptoms are actually secondary infections or complications arising from the initial measles infection. Accurate diagnosis requires careful clinical evaluation.
Identifying Risk Factors
Several factors increase the risk of developing persistent or complicated measles infections. These include:
- Immunocompromised individuals: People with weakened immune systems (due to HIV/AIDS, cancer treatments, or other conditions) are more susceptible to severe and prolonged measles infections.
- Malnutrition: Poor nutrition weakens the body's ability to fight off infection, increasing the risk of complications.
- Vitamin A deficiency: Vitamin A plays a crucial role in immune function. Deficiency increases the severity and duration of measles.
- Young age: Infants and very young children are particularly vulnerable to severe measles complications.
Understanding these risk factors allows for targeted preventative measures and earlier intervention in high-risk populations.
Medical Interventions for Combating Measles
Role of Supportive Care
Supportive care is crucial in managing measles symptoms and preventing complications. This involves:
- Hydration: Maintaining adequate fluid intake is essential to prevent dehydration, a common complication of measles, especially in young children. Oral rehydration solutions are often recommended.
- Fever management: Paracetamol (acetaminophen) can help reduce fever and discomfort. Avoid aspirin, which can increase the risk of Reye's syndrome.
- Nutritional support: A balanced diet provides the body with the nutrients it needs to fight infection. In cases of severe illness, nutritional support might require intravenous fluids.
- Monitoring for complications: Regular monitoring for signs of pneumonia, encephalitis, or other complications is essential for timely intervention.
Treatment of Complications
Measles complications require prompt and appropriate medical treatment. This can include:
- Pneumonia: Antibiotics are necessary to treat bacterial pneumonia, a common complication of measles.
- Encephalitis: Encephalitis requires specialized medical care, often including antiviral medications and supportive measures to manage brain swelling.
- Other complications: Other complications, such as otitis media (middle ear infection) or diarrhea, may require specific treatments depending on their severity.
- Specialist referral: Severe cases of measles requiring hospitalization and specialized care should be referred to a hospital with appropriate resources.
Prevention: The Key to Combating Future Measles Outbreaks
Vaccination Strategies
Measles vaccination is the most effective way to prevent measles infections and outbreaks.
- Recommended schedule: Most countries follow a two-dose vaccination schedule for children. The first dose is typically given at 6-12 months of age, and the second dose is given later in childhood. Consult your doctor for the exact schedule in your area.
- Herd immunity: High vaccination rates (at least 95%) are crucial to achieve herd immunity, protecting even those who cannot be vaccinated due to medical reasons.
Public Health Measures
Public health initiatives play a critical role in controlling measles spread:
- Surveillance: Monitoring measles cases to identify outbreaks and trends.
- Contact tracing: Identifying and monitoring individuals who have been in contact with infected persons.
- Quarantine: Isolating infected individuals to prevent further spread.
- Public awareness campaigns: Educating the public about measles prevention, symptoms, and the importance of vaccination.
Effective public health measures are essential for preventing and controlling measles outbreaks, especially in communities with low vaccination rates.
Conclusion
Combating measles requires a multi-pronged approach. Supportive care for those already infected, prompt treatment of complications, and, most importantly, widespread vaccination are vital. Persistent measles infections, though relatively rare, highlight the seriousness of this preventable disease. Together, we can effectively combat measles and prevent persistent infections. Protect yourself and your community: talk to your doctor about measles vaccination and ensure you're up-to-date on your immunizations. Let's work together to eradicate measles.
Featured Posts
-
 Harvard And The Trump Administration A Clash Of Ideologies
May 30, 2025
Harvard And The Trump Administration A Clash Of Ideologies
May 30, 2025 -
 Key Deutsche Bank Executive Jumps Ship To Morgan Stanley
May 30, 2025
Key Deutsche Bank Executive Jumps Ship To Morgan Stanley
May 30, 2025 -
 The Housing Market Crash Experts Report Crisis Levels In Home Sales
May 30, 2025
The Housing Market Crash Experts Report Crisis Levels In Home Sales
May 30, 2025 -
 Augsburg Bayern Muenih Canli Mac Yayinini Bulma Rehberi
May 30, 2025
Augsburg Bayern Muenih Canli Mac Yayinini Bulma Rehberi
May 30, 2025 -
 Manila Bays Ecosystem Challenges And Opportunities For Sustainability
May 30, 2025
Manila Bays Ecosystem Challenges And Opportunities For Sustainability
May 30, 2025
